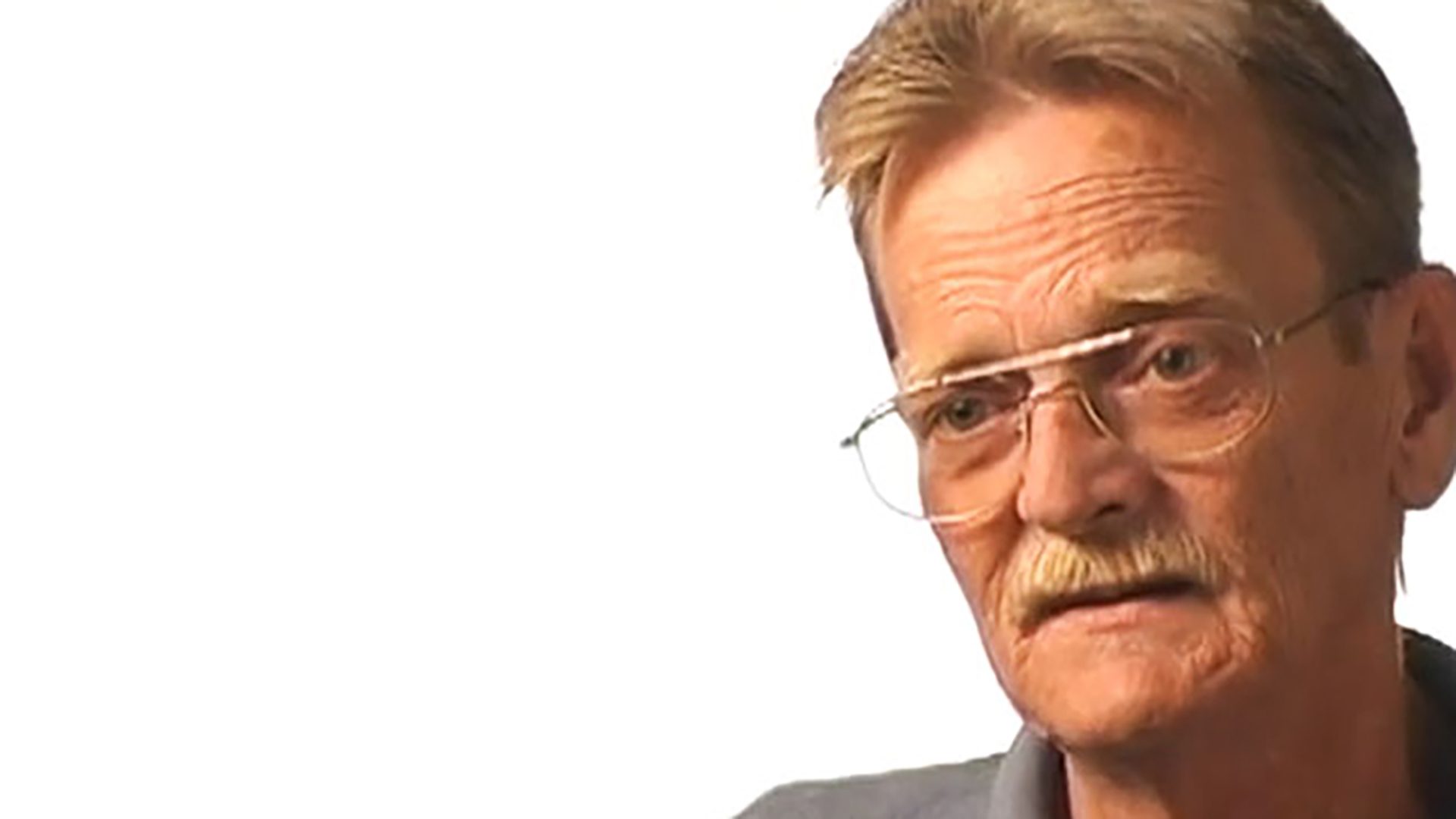
Survivor Interview – Laura B.
Laura is a breast cancer survivor. She talks about hospice, planning her financial and medical future, and how she deals with fear of recurrence.

I became a breast cancer survivor when I was diagnosed in 1997.
For people that think that having a mammogram makes them okay for a year, that’s really not the case. I had a mammogram in April and everything was fine. But in June, I discovered a lump as I was taking off my makeup. Immediately, I rushed to the physician the next day and had it checked out. He did a needle biopsy and found some abnormal cells, and then referred me to a surgeon. Having had a lot of the biopsies before in the past, I thought it would just be a little breast biopsy. It would be a benign cyst and everything would be fine. I got to the surgeon’s office and he started talking about mastectomies and cancer. I thought, “Why are we having this conversation?” He looked at me and said, “You’ve not seen your pathology report, have you?” I said, “No,” and he showed it to me. That’s when I saw the word “malignant.” It really took me aback, because that’s always something that you think happens with other people and not you.
I had the lumpectomy and then went right on in to six treatments of chemotherapy. I did radiation following the chemotherapy. Fatigue was something that I dealt with a lot, which is very common. For people going through those type of treatments, you have to learn to listen to your body. When it says, “We need to jump off the merry-go-round, and take a nap,” then you take a nap. Oftentimes, you can’t argue with your body because it just shuts down. A lot of dryness in my skin seemed to be one of the more irritating things. I felt like my skin was sandpaper. My fingers and my face got extremely dry. I just drank up the moisture. I remember having to put on things like massage creams, which are real thick and heavy, simply because that was the only thing that would give me any relief from that.
I think having a good attitude about the whole thing has been really key for me. A lot of women that face these kinds of things often have a fear of, “Oh, my gosh. When is it going to happen again?” Dreading that next mammogram. Dreading possibly feeling another lump and the prognosis that may result as a result of that. But that’s not something that I’ve really spent a lot of time worrying about because you can waste a lot of today’s worrying about tomorrow. I really don’t believe that that’s a productive way to live. You may not be able to control the actual multiplication of the cancer cells that may or may not be happening. But there are things you can do as far as taking care of yourself whether it’s healthy eating, exercise, mental attitude – I think that is critical. Having that support system within your family or your friends is so important to positive outcomes that are out there. I believe that truly, people need to live every day of their lives and not worry about something that may or may not be happening down the road.
When trying to get any kind of supplemental life insurance or health insurance, nobody wants to even look at you until you’ve been cancer-free for at least ten years. Those aren’t always issues that you think about when you’re younger. You think, “I’ve got enough insurance. I’m going to live forever. I’ll be healthy.” But when that threatens, you start thinking, “I might need to increase some of my coverage here,” and that’s been a really big issue with me – just not being able to have access to more coverage until you wait out that time period for them. Any time you change employers, you face that change again. When I was diagnosed, I was working for a pharmaceutical company. I had really good life insurance and health insurance coverage. But don’t take those for granted because when I made a career change to the hospice industry, sometimes your choices change as well. You see the need that, “Maybe I do need to supplement the coverage that I’ve had in the past.”
People need to be proactive in finding things on their own and not just relying on their physician or the nurse to tell them things about cancer. Going on the Web, doing a lot of research on your own. When people are facing crisis in their lives, there are a lot of predators out there that-through false information or products-take advantage of people, and you have to be careful of that. Ask questions. Sometimes people are afraid to ask questions because they don’t want to hear the answers. But if you don’t ask, you don’t know. Knowledge is so powerful, especially in this cancer diagnosis. Things are changing every day. It’s exciting to see some of the things that are happening. But you do need to filter the information that you’re getting and try to be sure that you are getting them from some valid resources.
Death and dying is often a difficult conversation to have because people don’t want to actually admit that they’re facing end-of-life issues. My mother had breast cancer twenty-five years before she had a recurrence. It recurred in the lining of her lungs. We had taken her to several different oncologists to get second opinions. When it was confirmed that the disease was progressing, and there really wasn’t anything that could be done to slow the progression of the disease, the decision was made to call in hospice.
At the time, I didn’t realize the full benefit that hospice offers. If a person is Medicare-aged, hospice is truly a one hundred percent earned benefit. They cover everything from medications and equipment to nursing services. There is a whole support team that is out there. This was a huge help because my dad was trying to care for my mom in the home. We daughters were all living in the Central Texas area and in the Panhandle. We would fly in on the weekends, but during the week, there was nobody in there to help him share that load in caring for her. She also developed Alzheimer’s at the same time. So you had both the mental and the physical aspects that were going on with her diseases.
Hospice would come in once a day. A nurse’s aide would help bathe her, and give my dad that break, even if he just wanted to walk outside and take a breath and not feel like he was on-duty for that hour or so that they were there. Having somebody else help with her bathing, washing her hair and having that additional support, whether it was the chaplain coming in to talk with him, and just let him know that, “You’re not having to do this by yourself. We’re all here with you.” Also knowing that you have that lifeline that you can call anytime of the day, whether it’s 3:00 in the morning or 10:00 at night, there is always somebody there if you needed them to come, they could. That was a huge relief knowing that there was somebody there to help our dad with our mom, especially during that time when we couldn’t be there. We augmented that with a lot of the friends and family members that were also there to help with her care.
That was a huge gift to our family. At the time, I always thought, “One of these days, I want to do something to be able to give back to this organization.” I never dreamed I would be fully employed with them. It’s been nice to see how everything has come full circle, where I am able to take the experiences that I have had personally as a recipient of the care-giving that hospice provided. And then being a survivor myself and knowing some of the situations that people are facing. It has allowed me to be able to share with people that are facing these issues.
I think it is important that people have their affairs in order. That is just a practical thing to think about, but that is not something that we all really want to take the time to deal with. Having a will. Letting your family members know what your desires are, what you want to have happen. Maybe it is wishes that you want to have as far as organ donation goes. Maybe it is having a foundation set up for educational funding for your children. Maybe it is just knowing where your loved one wants to spend their last days, hours, months of their life and how they want that to happen. Most people want to be where they call “home” whether it is in their home, a nursing home, or in assisted living. That’s where most people want to be, surrounded by things that are familiar and that they love. That often gives the family members time and access to that patient more frequently than going to a hospital setting or an inpatient setting, and to have visitation hours. It really gives them that interaction with that loved one, that 24 hours a day, which is really neat to have happen.
To me, Livestrong means to live life with a zest for living. Living every day of your life is important, and we need to do that with a strength and a powerful conviction that we are living each day to the best of our ability.
My name is Laura Bennett, and I’m an eight-year breast cancer survivor.