Osteoporosis
Osteoporosis is a condition that causes your bones to weaken and become very fragile—sometimes fracturing with little or even no impact. Primary osteoporosis happens from the normal process aging and/or menopause. Secondary osteoporosis is something survivors can experience as a side effect of cancer and treatment.
Osteoporosis is sometimes called “a silent disease” because it can exist for years without symptoms — until a bone is broken or fractured. The condition is treatable, but not curable. It’s important to be aware of your risks for developing osteoporosis. This can help you detect symptoms early and get effective treatment.
Risk Factors for Osteoporosis
Cancer types:
- Breast cancer.
- Prostate cancer.
- Multiple myeloma (cancer that occurs in the antibody-producing white blood cells).
- Other solid tumor types such as lung, testicular, ovarian and endometrial (uterine wall) cancers.
Cancer treatments:
Treatment for some cancers, such as breast or prostate cancer, can include blocking or eliminating certain hormones in your body. Blocking sex hormones (testosterone or estrogen) helps to slow the growth of cancer cells. However, the sex hormones also protect the bones. If your body is deprived of these hormones, osteoporosis can develop. If you received or will receive this type of treatment, talk with your health care provider about things that can be done to prevent or minimize bone loss.
If you develop osteoporosis, it does not mean that your health care team did a bad job. The primary goal of your health care team is to treat your cancer in the most effective way possible. After treatment, their job is to work with you to manage aftereffects you might experience.
Lifestyle and other risk factors:
- Health problems such as hyperthyroidism, rheumatoid arthritis or diabetes.
- Family history of breast cancer.
- Small body frame or low body weight.
- Advanced age.
- Being female–osteoporosis is more likely to occur in women, especially after menopause.
- Ethnicity–Caucasians and Asians generally have a higher risk.
- Low testosterone levels in men.
- Certain medications that are taken for a long time.
- Low intake of calcium and vitamin D.
- Too much caffeine.
- Inactivity or too little exercise.
- Smoking.
- Drinking too much alcohol.
Minimize the Risks for Osteoporosis
Osteoporosis can be minimized and controlled, but not cured. This means that once you know you have this condition, you can work with your health care team to develop ways to slow down any bone loss. Here are some ways to help minimize your risk of developing osteoporosis:
- Stop smoking.
- Drink little or no alcohol.
- Exercise.
- Maintain a healthy weight.
- Include calcium, Vitamin D and Vitamin K in your diet.
- Limit caffeine and Vitamin A.
- Avoid falls.
- Talk with your health care provider about medications that can help decrease bone loss.
- Discuss alternative therapies with your health care team.
Symptoms and Signs
Bone loss related to osteoporosis typically happens slowly over time. A person can have osteoporosis and not experience any symptoms. Talk with your health care provider if you think you’re at risk for osteoporosis. Ask about screening tests for osteoporosis. Some symptoms of osteoporosis may include:
- Weight loss.
- Stooped posture.
- Curving of the upper back (Dowager’s hump).
- Bone tenderness.
- Loss of one or two inches in height.
- Bone break or fracture.
If you experience any of these symptoms, it doesn’t always mean you have osteoporosis. Discuss your concerns with your health care team.
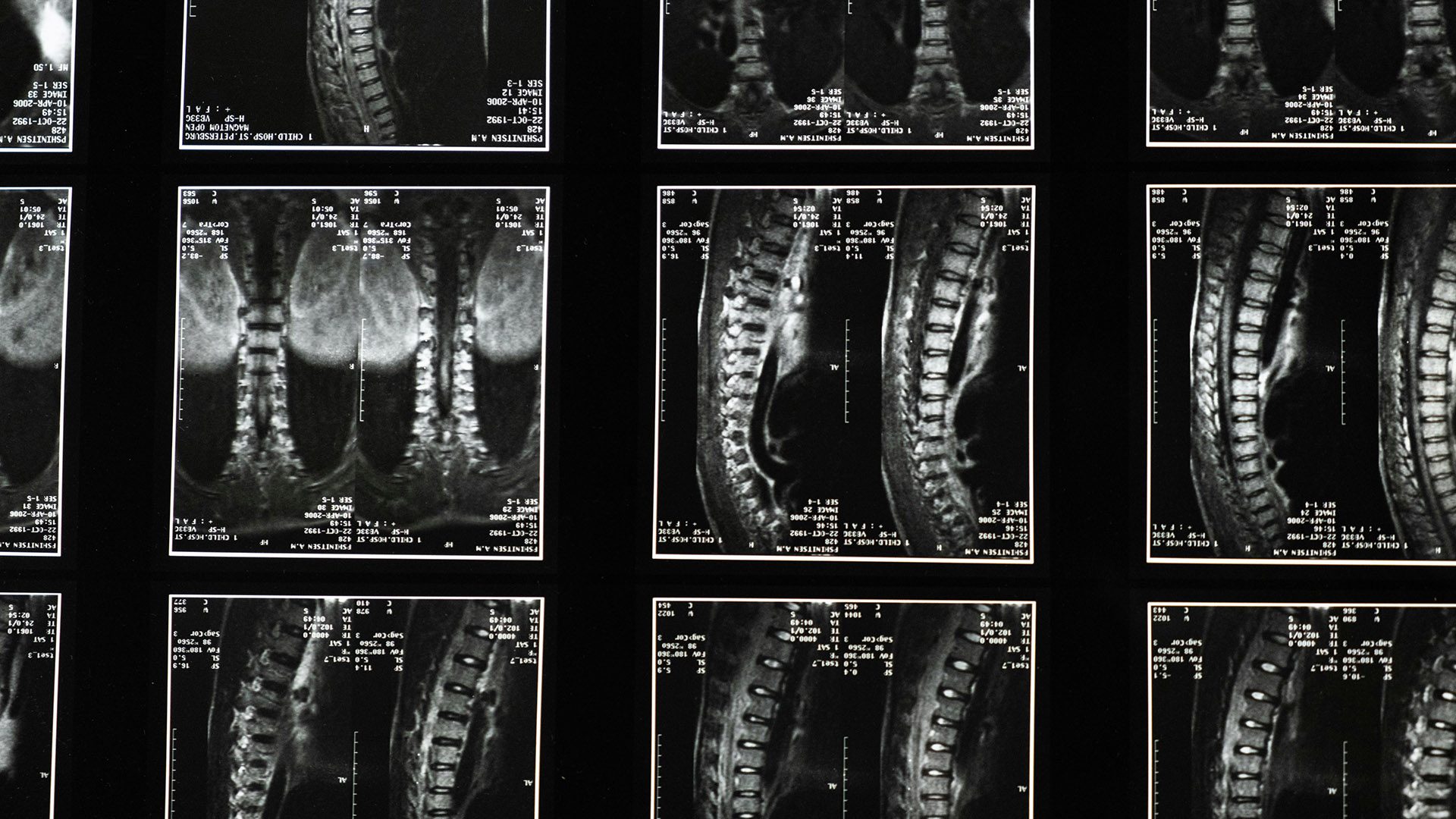
Testing for Osteoporosis
The most common and widely used test for osteoporosis is called the DEXA (dual energy x-ray absorptiometry) scan. It measures the amount of calcium in bone, typically at the hip and lower spine. It’s recommended for individuals who may be at risk for osteoporosis, such as women who are 65 or older and men who are 70 or older, some cancer survivors, and anyone over the age of 50 who has a newly fractured bone.
The DEXA scan should be repeated every couple of years to check whether your bone density has changed. Your T-score compares your results to healthy bones of young adults. The following table shows the range of T-scores that are used to assess risk:
| Normal T-score | -1 to +1 |
| Osteopenia (pre-osteoporosis) | -1 to -2.5 |
| Osteoporosis | -2.5 or lower |
| Severe osteoporosis | -2.5 or lower with one or more fractures |
Osteopenia is diagnosed when the bone mineral density is lower than normal. Many health care providers think that it may be a precursor to osteoporosis. However, many people diagnosed with osteopenia never develop osteoporosis.
Talk with your health care team about your risk for developing osteoporosis. It usually happens after age 65. However, it may happen sooner if you received treatment that puts you at high risk for bone loss. The more risk factors you have, the higher your chances of developing osteoporosis at some point during your life.